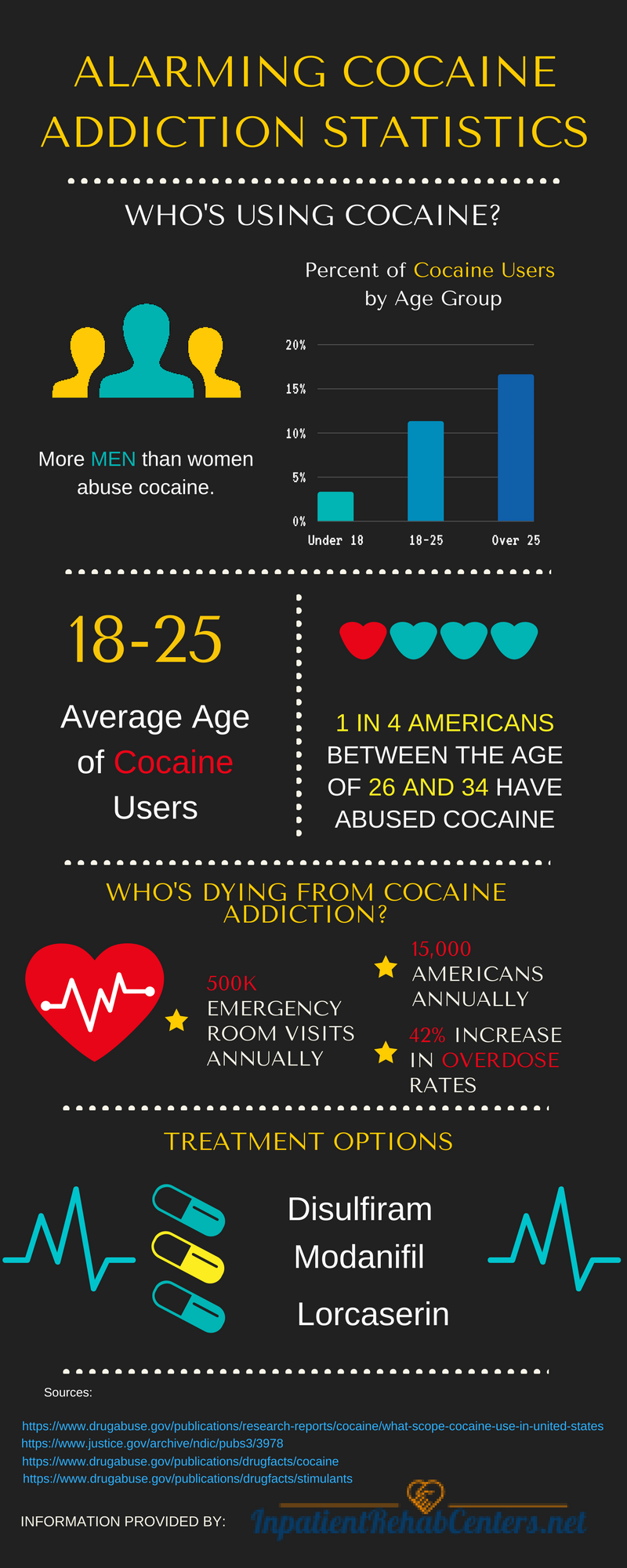
People tend to minimize the risks associated with cocaine, overlooking entirely the risk of overdose. But, cocaine is extremely dangerous and even first time users are at grave risk of overdose.
If you are struggling with cocaine addiction, your chance of overdose increases dramatically because you are using the drug more frequently. Unfortunately, many people do not survive cocaine overdoses; according to the National Institute on Drug Abuse, cocaine overdose deaths increased 42 percent between 2001 and 2014. Those who survive an overdose may find it is the wake-up call they needed to deal with their cocaine addiction and often FINALLY make the decision to seek treatment in an inpatient rehab.
Why Do People Overdose?
There are obviously a lot of situations that lead people to overdose, but all of them have to do with using too much cocaine in order to get high or to maintain a high. For example, some users continue to abuse the drug while there are still large amounts of cocaine in their system and this multiplies the effects of the drug. Other users may take a large dose because they have developed a tolerance and can’t achieve the same high with their old dose.
Often times, cocaine overdose is a complete accident. Users may obtain a drug that is much stronger than what they are accustomed to getting and not realize the risks when they use. If a drug has a higher potency or purity than what a user is accustomed to overdose can quickly happen without notice.
If you or someone you love is abusing cocaine, don’t wait until an overdose occurs to seek help. Call 1-800-559-0697 today to find an inpatient rehab center near you.
What Are the Signs of Overdose?
Common signs that someone has used too much cocaine may include:
- Aggression
- Paranoia
- Panic attacks
- Severe mood changes
- Anxiety
- Irritability
- Extreme levels of energy
- Abdominal pain, nausea, vomiting
- Headache
- Raised body temperature
- Increased blood pressure
- Increased heart rate
- Fainting and/or dizziness
- Chest pain
- Seizures
- Coma
What Do I Do If Someone Is Overdosing?
Cocaine affects many of the user’s bodily systems and an overdose can quickly turn fatal if left untreated. For example, the arteries that feed the heart may constrict, starving the heart of oxygen. This can lead to a deadly heart attack or stroke that provides little to no notice before medical attention become vital.
If you suspect that an overdose of cocaine has occurred it is important to immediately call 911. While you are waiting for an ambulance:
- Use cold compresses to reduce elevated body temperature
- Move furniture and items out of the way in case of seizure
- Remain present until help arrives
If there is no immediate emergency of overdose, but someone you love recently overdosed or you suspect that cocaine overdose risks are possible, call 1-888-605-7779 for help finding an inpatient rehab center.
Trying to Get Clean
After a potential overdose, you may decide enough is enough and it’s time to really focus on getting clean. If this sounds like your current situation, know first that you are NOT ALONE. Thousands of people struggle with cocaine addiction and need help. Many try several times to get clean before they seek professional help- and that’s “ok.”
Cocaine withdrawal is a real risk if you attempt to quit using after a prolonged period of use. In fact, many users struggle for months with underlying symptoms of cocaine withdrawal trying their best just to get well and feel better.
What Are the Symptoms of Cocaine Withdrawal?
Stimulants such as cocaine produce withdrawal symptoms that are unlike those caused by sedatives, opioids, or alcohol. According to the Substance Abuse and Mental Health Services Administration symptoms of withdrawal from cocaine may include:
- Drug cravings
- Irritability
- Paranoia
- Anxiety
- Increased appetite
- Fatigue
- Psychomotor retardation
- Hypersomnia or insomnia
- Poor concentration
- Depression
Cocaine withdrawal rarely produces intense discomfort or medical danger. However, if a specific patient exhibits signs of a poor outcome during detox, clinical interventions may be used.
Typically, symptoms of withdrawal from cocaine clear up after several days, but they can continue for 3 to 4 weeks or longer depending on the severity of the addiction and the length of time the drug was used.
Dangers of Cocaine Withdrawal
Many overlook the dangers associated with dysphoria (negative thoughts and feelings), but this is the most commonly cited cocaine withdrawal symptom that can be potentially fatal. Experts believe that dysphoria is a combination of \ withdrawal effects from stimulants such as cocaine coupled with the dawning realization of the consequences that have resulted from a binge. Together, these components can lead to suicidal thoughts and attempts.
Addicts may also face cardiac complications; therefore, IF withdrawal is taking place in a controlled medical detox facility the detox staff are to be made acutely aware of chest discomfort and any potential cardiac symptoms.
Another serious danger, seizures. It is common for seizures to occur during cocaine withdrawal. If someone you love is struggling with cocaine addiction, these dangers are some of the most common reasons why it is highly recommended that you seek professional treatment in an inpatient rehab center or detox center.
For help finding an inpatient rehab that can help you or your loved one overcome cocaine addiction, call 1-888-605-7779 today.
Safe Withdrawal in a Detox Center
The most effective method of safe withdrawal from cocaine is through the establishment of a period of abstinence. Intensive outpatient detox can generally accomplish this. If a patient can stay clean long enough, negative symptoms usually stop on their own. There are no medications approved by the Food and Drug Administration for treating cocaine withdrawal.
Cocaine Addiction Treatment
Cocaine dependence and addiction are crippling, but there are many treatment options available. Help is accessible IF you’re ready and willing. Inpatient rehab can help you or your loved one to get sober once and for all.
If you’re ready to overcome cocaine addiction, call 1-888-605-7779 today to find an inpatient rehab center near you.
Inpatient vs. Outpatient Rehab
If you choose inpatient rehab, you will be required to live at the rehab center. This is a great option for people who need the security of a drug and alcohol free environment. It also benefits addicts by separating them from the triggers and stressors that they encounter in their daily life.
Outpatient treatment only requires visits to the rehab center when there is a scheduled treatment meeting or therapy session. This option works well for people who cannot take time away from their responsibilities at home or work and it may also be less expensive.
Both options can work wonderfully for those struggling with cocaine addiction. The one that will work best for you is determined by your specific situation.
Behavioral Therapy
Psychological approaches that address the motivations, thinking, and underlying psychological issues that contribute to a pattern of substance abuse are the primary focus of behavioral therapy. By dealing with these underlying factors of addiction, counselors and therapists enable patients to make positive changes in their lives.
One type of behavioral therapy commonly used in cocaine addiction treatment is contingency management. This is a treatment that uses tangible incentives (cash or prizes) to encourage positive behaviors. Much like abstinence and improved social interactions, contingency management has proven effective for many people with cocaine addictions.
Pharmacological Therapy
In addition to behavioral treatment options, many pharmacological or medicine-based approaches are available to treat cocaine addiction. While there are currently no medications approved by the FDA for the primary purpose of treating cocaine addiction or dependence, there are a wide range of medications that can be used to help reduce symptoms of withdrawal such as anxiety, depression or insomnia. Many of these same medications are sometimes used long term as the user’s hormonal balance returns to a normal state.
Emerging methylphenidate treatment is also proving effective. Typically used to treat attention deficit hyperactivity disorder, this drug is sort of like cocaine. It causes the brain to feel as if any existing cravings have been satisfied without the user actually getting high.
Finding Inpatient Rehab
If you’re ready to get sober, or you know someone that’s struggling with an addiction to cocaine and needs help, consider calling 1-888-605-7779 to find a local rehab center near you. As you’ve seen, many therapeutic options are available to help you or a loved one to balance out and feel better despite an addiction to this powerful stimulant. One call could literally save your life…don’t delay, get the help you need today.















































 The results of a recent study have found that heavy marijuana use may decrease the level of dopamine released in the brain. Dopamine is a chemical transmitter that sends signals to the brain and is involved in movement, as well as learning, memory, cognition and pleasure.
The results of a recent study have found that heavy marijuana use may decrease the level of dopamine released in the brain. Dopamine is a chemical transmitter that sends signals to the brain and is involved in movement, as well as learning, memory, cognition and pleasure.